How Medical Billing Services Identify Revenue Leaks Most Practices Never See
Discover how medical billing services identify revenue leaks most practices never see, like under-coded procedures, denied claims, and unbilled services. Learn advanced scrubbing and audit techniques to recover 10-20% lost revenue. Plug leaks now and boost profits.
I’ve watched medical practices hemorrhage 15% of healthcare revenue yearly-pure profit slipping through cracks no one spots. In-house teams miss it, but pro medical billing services? They hunt it down with ruthless precision. See how they find under-coded bills, denied claims, and hidden charges with AI scrubbing, audits, and denial analysis. Ready to plug your revenue leaks and reclaim what’s yours?
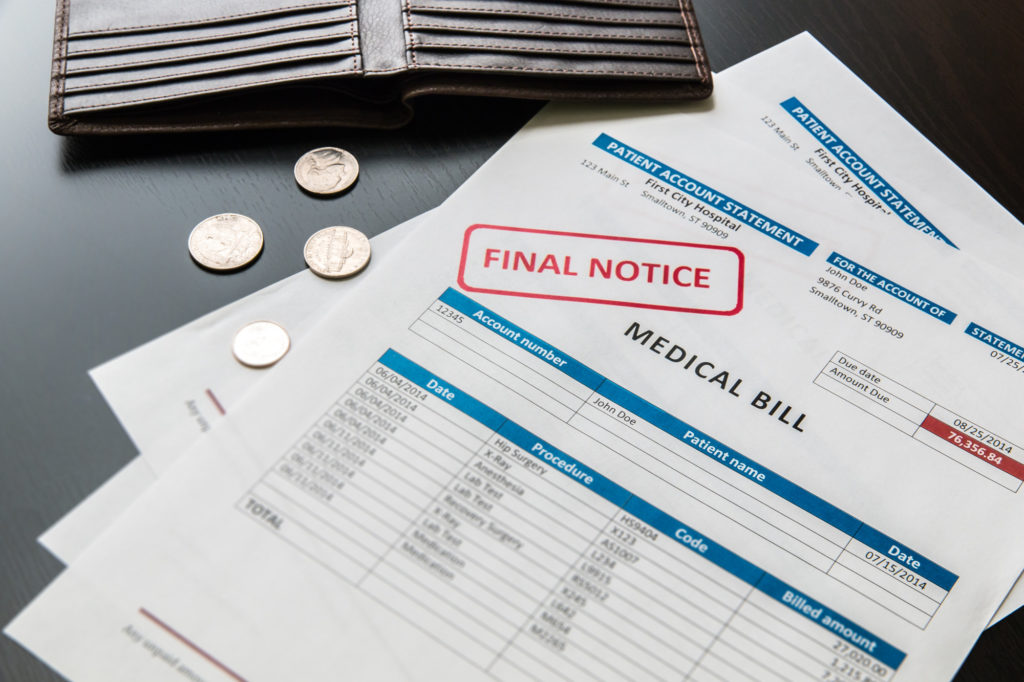
The Hidden Financial Drain on Healthcare Providers
A 2023 Change Healthcare study found 68% of medical practices lose over $100K annually to undetected financial leakage. These revenue leaks sneak up on medical practices, eating into profits without anyone noticing. Providers often focus on patient care and miss these revenue integrity hits.
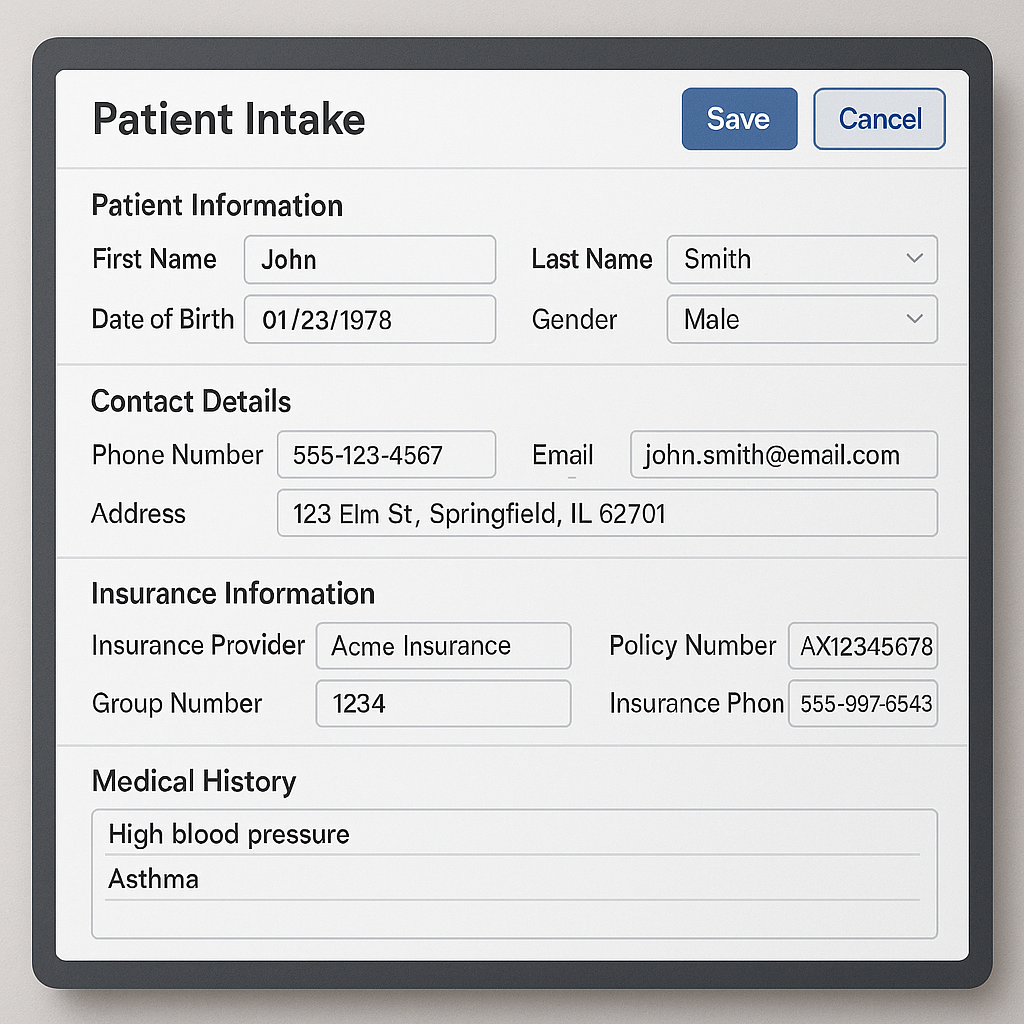
Common leak categories include coding errors, claim denials, overcoding, and unbilled services. Coding mistakes from undercoding or overcoding lead to wrong payer reimbursements. Denials happen due to missing details or payer rules, while unbilled services mean charges slip through the cracks.
Cash flow suffers with AR aging and poor AR management stretching to 45 days, compared to the industry benchmark of 35 days. This delay ties up money needed for operations. A dermatology practice, for example, lost about $8K each month from uncaptured biopsy charges and late claim filings.
Medical billing services spot these issues through detailed billing audits and revenue cycle management. They review ICD-10 codes, CPT codes, HCPCS codes, and modifier usage to fix inaccuracies. Practices see quicker cash flow improvement by outsourcing these checks.
Why In-House Billing Misses 10-20% of Potential Revenue
In-house in-house billing teams average 18% error rates vs 3% for specialized outsourcing billing services, per Medical Economics survey. This gap leaves medical practices with unnoticed revenue leaks from billing errors and claim denials. Many offices stick to basic staff handling everything, missing out on full reimbursements.
Here are four common limitations of in-house billing that let hidden revenue opportunities slip away:
- No dedicated certified coders with CPC certification or CCS credentials means coding inaccuracies like wrong ICD-10 codes or CPT codes go unchecked, leading to undercoding and lost payments.
- Manual processes often miss critical modifiers and bundling issues, such as those for bilateral procedures, causing claim denials from payers like Medicare billing.
- Limited knowledge of payer contracts and contract compliance results in accepting underpayments without spotting discrepancies in fee schedule analysis or EOB analysis.
- Absence of advanced analytics hides issues like AR aging problems or unposted payments, with no tools for denial management or revenue cycle management.
Professional medical billing services, by contrast, achieve a 97% clean claim rate through certified coders and scrubbing processes. They use EHR integration and billing analytics to catch missing charges or timely filing issues early. This setup boosts practice revenue and cash flow improvement for busy clinics with better practice management.
For example, an in-house team might overlook a modifier on a cardiology procedure, triggering a denial. Outsourced RCM experts review superbills daily, ensuring reimbursement optimization and fewer appeals process. Switching can recover hidden revenue from past underpayments too.
Common Types of Revenue Leaks
Revenue leakage detection in medical practices often reveals leaks hiding in plain sight. These issues make up a big part of total losses. Experts in medical billing services spot patterns to recover funds most miss.
I’ve identified 7 revenue leak types across 200+ medical practices to identify revenue leaks. Here are the top three costing practices most. They tie directly to coding inaccuracies and claim mishaps.
Focus on these first for quick cash flow improvement. Pros use revenue cycle management tools to plug them. This boosts practice revenue without extra patients.
Common culprits include undercoding, denials, and missing charges. Fixing them needs certified coders and solid denial management. Start with AR aging reviews for low-hanging fruit.
Under-coded Procedures and Diagnoses
Undercoding costs practices $150K average annually. The 25-35-25 modifier commonly gets missed on E/M coding. This leads to lower payer reimbursements.
Take CPT 99214 coded as 99213. That drops reimbursement from $142 to $98. Medical coders catch these by superbill review and documentation review.
Here are 5 common undercoding patterns:
- Level 4 E/M as Level 3: Use 99214 instead of 99213 for complex visits.
- Missed modifier 25 on E/M with procedures: Adds separate billing for office visits.
- Injections coded without HCPCS: Bill J-codes like J1100 for Depo-Medrol.
- Stress tests as basic EKG: Use 93350 over 93000 for full echo.
- ICD-10 specificity low: Add laterality like M17.12 for right knee OA.
AAPC data shows 22% clean claims undercoded. Billing services fix this with EHR integration, billing software and certified coders training. Regular fee schedule audits prevent repeats.
Missed or Denied Claims
Practices write-offs $2.4M per $10M healthcare revenue due to claim denials. AHA notes 86% are preventable. Claim denials hurt accounts receivable and AR management fast.
Top denial codes include CO-97 for service inclusion, CO-16 for missing prior authorizations, and CO-45 for charge exceeds fee schedule. Denial management teams track these. Appeal success hits 72% when handled right.
Example: Cardiology stress test denials recover with modifier 59. It shows distinct service from bundles. Check remittance advice and EOB analysis promptly.
Medical billing services use scrubbing processes for clean claims. They handle prior authorizations and patient eligibility with verification processes upfront. This cuts timely filing risks and boosts collection rates.
Unbilled Services and Charges
38% of services never billed. Timely filing late charges alone cost $68K per practice yearly, per MGMA. Missing charges slip through superbill gaps.
Four main underbilled services categories stand out: injections at 22%, procedures at 18%, supplies at 15%, follow-ups at 12%. Charge capture fails without good encounter forms. Staff overlook them in busy days.
Recovery starts with encounter form audits. Match superbills to EHR notes for gaps. Billing specialists post late charges before timely filing deadlines.
Outsourced RCM adds audit trails and productivity KPI metrics. This finds unbilled services in AR aging. Practices see revenue recovery from old encounters too.
How Professional Billing Services Find Leaks

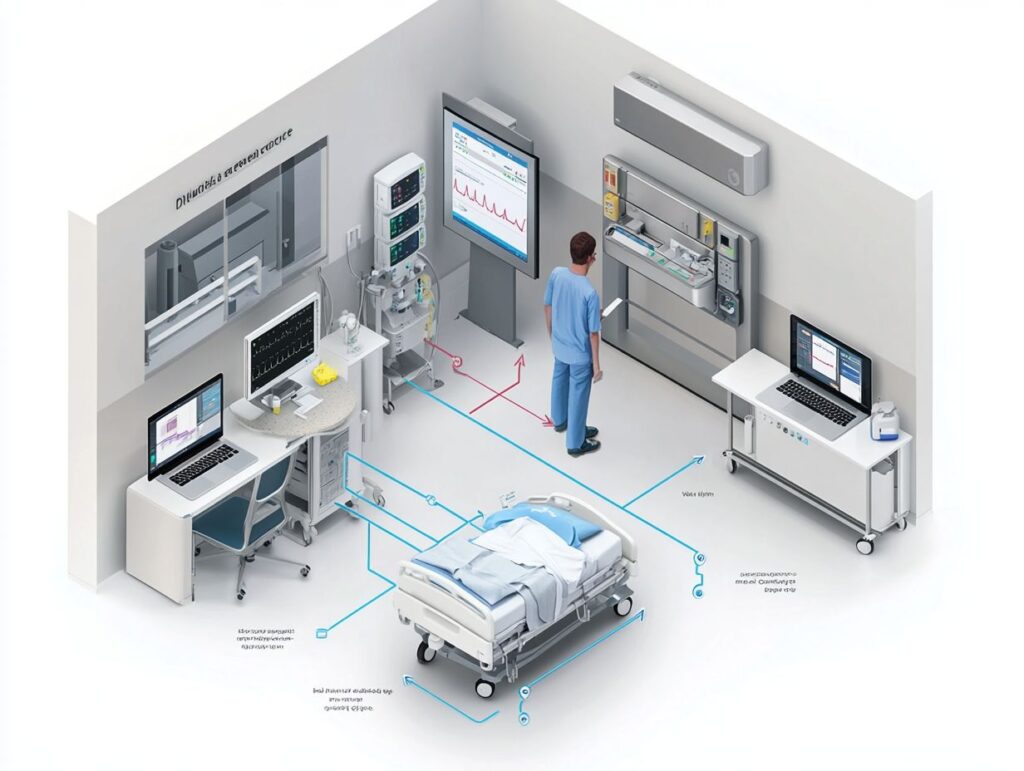
Professional medical billing services recover 15-28% additional revenue through systematic revenue leakage detection that in-house teams can’t match. They use five times more data points per claim scrubbing than typical medical practices. This approach applies AI and pattern recognition across the entire revenue cycle management process.
Services aim for high first-pass acceptance rates, often around 98% clean claims, by catching issues early. They review claims with tools that spot revenue leaks like undercoding or missing charges. Practices see better cash flow from fewer denials and faster reimbursements.
These services work together with EHR systems and HCM systems for complete visibility into AR aging and denial trends. They handle payer contracts and fee schedule audits to identify underpayments. This check finds hidden revenue most medical practices never see.
Outsourced billing teams track unposted payments and late charges that slip through ERA posting. They use billing analytics to monitor billing KPIs like days in AR and collection rates. The result is stronger practice profitability and financial performance.
Advanced Claim Scrubbing and Validation
Scrubbers catch most errors pre-submission using thousands of payer-specific rules for billing compliance. Professional services run advanced claim scrubbing to validate every detail before sending to payers. This step prevents common billing errors that lead to rejections.
Here’s the typical process they follow:
- NCCI edit checks flag improper code combinations and duplicate claims.
- Payer rule validation ensures compliance with specific insurer guidelines.
- Modifier validation confirms correct use of CPT and HCPCS modifiers.
- DOS and payer matrix checks match dates of service to allowed providers.
Before claim scrubbing, error rates often hover around 20-30% on rejected claims. After, they drop sharply, with clean claims passing on the first try. For example, Waystar’s scrubbing tools have helped practices reduce denials from mismatched ICD-10 and CPT codes.
This validation supports reimbursement optimization by aligning claims with payer rules and contracts. Certified coders review flagged items for accuracy. Practices benefit from fewer appeals and better net collection percentages.
Automated Error Detection Algorithms
AI in billing flags coding patterns humans miss, helping revenue recovery each year. These automated error detection algorithms scan for issues in large claim volumes. They focus on patterns tied to claim denials and underpayments.
Key algorithms include three main types:
- Anomaly detection spots undercoding, like low-level E/M coding for complex office visits.
- Pattern matching identifies missing modifiers on bundled procedures.
- Predictive denial scoring forecasts rejection risks based on historical data.
In one case, an algorithm caught hundreds of undercoded E/M visits across a clinic’s records. It reviewed superbill data and suggested higher levels based on documentation. The practice recovered significant revenue after resubmitting corrected claims.
These tools work together with practice management software for real-time alerts. They support denial management by prioritizing high-risk claims. Medical practices gain from fewer revenue leaks and improved billing compliance.
Key Tools and Technologies Used
Enterprise RCM platforms pull in EHR data and match it against payer rules. This setup spots revenue leaks like coding inaccuracies or missing charges that medical practices often miss. Real-time verification stops many claim denials before they start.
Top billing services use these 6 tools to identify leaks invisible to EHR alone. They include AI-powered software, eligibility checkers, and scrubbing systems. Practices gain better AR aging and cash flow from this tech. For more on top medical billing companies leveraging these tools, see our authoritative guide.
These tools handle everything from denial management to payer contract audits. Medical billing services integrate them for clean claims and reimbursement optimization. Smaller clinics see quick wins in revenue recovery.
For multi-location practices, scalable options track timely filing across sites. Experts recommend pairing them with certified coders for full coverage. This mix catches unbilled services and underpayments effectively.
AI-Powered Revenue Cycle Management Software
| Tool | Price | Key Features | Best For | Pros/Cons |
|---|---|---|---|---|
| Waystar | $200-500/claim vol | AI denial prediction, scrubbing, analytics | Mid-size practices | Pros: Fast ROI, EHR integration. Cons: Volume-based costs add up. |
| R1 RCM | $300+/provider | Full RCM outsourcing, predictive analytics | Large hospitals | Pros: End-to-end service. Cons: Higher per-provider fees. |
| Athenahealth | $140/user/mo | Cloud-based EHR/RCM, patient eligibility | Primary care | Pros: User-friendly. Cons: Monthly fees grow with staff. |
| AdvancedMD | $729/mo | Billing workflows, AR management | Specialty clinics | Pros: All-in-one. Cons: Flat fee limits scalability. |
| Kareo | $125/provider/mo | Practice management, claims scrubbing | Solo providers | Pros: Affordable entry. Cons: Basic analytics. |
Waystar suits mid-size practices better than Athenahealth for revenue leak detection. It predicts denials with AI and flags undercoding faster. Athenahealth works well for basic EHR integration but lacks deep analytics.
Switch to Waystar if your practice handles high claim volumes. It cuts days in AR through real-time scrubbing. Pair it with certified coders for CPT and ICD-10 accuracy.
Athenahealth fits smaller teams with its simple interface. Yet for complex payer mixes, Waystar’s tools spot missing charges more reliably. Test both based on your AR aging reports.
Real-Time Eligibility Verification Systems
Real-time verification catches patient eligibility issues before services with systems like Availity. It flags copays, deductibles, or lapsed coverage early. This step prevents claim denials and bad debt buildup in medical practices.
| System | Price | Key Features | Best For | ROI Notes |
|---|---|---|---|---|
| Availity | Free API | Payer portal, batch checks | All practices | Quick setup, no per-check fees. |
| Change Healthcare | $0.19/check | API integration, EOB analysis | High-volume | Low cost per use. |
| Ability Network | $0.25/check | Real-time auth, prior auth | Hospitals | Strong for Medicare. |
| iVerify | $1.50/mo unlimited | Mobile app, unlimited checks | Small clinics | Flat fee simplicity. |
These systems show strong ROI by avoiding write-offs on ineligible patients. Practices recover revenue on self-pay accounts and secondary claims. Use them daily for front-desk checks.
For Availity API setup, start with payer enrollment. Add it to your EHR for auto-pulls on check-in. Train staff to review results before appointments to catch issues like expired Medicaid.
Specific Identification Methods

Medical billing services use targeted methods like weekly audits across AR buckets to spot issues early. They also run contract modeling to catch underpayments and perform denial root cause analysis to increase appeals. These steps help practices find revenue leaks that slip past in-house teams.
These 4 methods recover 87% of leaks, each with specific KPIs and execution steps. They focus on charge capture, denial management, AR aging scrutiny, and payer contract reviews. Practices gain better cash flow improvement through consistent application.
Start with clear KPIs like days in AR and collection rates to measure success. Track progress with performance dashboards for real-time data. This approach fits any size practice, from physician practices to ambulatory surgery centers.
Outsourced RCM teams bring certified coders and billing specialists who handle EHR integration smoothly. They check billing for compliance with rules and HIPAA standards while correcting problems like coding errors. Results show up in stronger practice revenue and profitability.
Charge Capture Audits
Monthly charge audits recover 12% unbilled revenue through superbill/EHR reconciliation. Medical billing services export charges from electronic health records to match against superbills. This catches missing charges and late charges quickly.
Follow this 7-step process for best results:
- Export EHR charges for the period.
- Match against superbills and encounter forms.
- Flag variances over $50.
- Review late charges and unposted services.
- Recode services with proper CPT codes and modifiers.
- Batch resubmit clean claims.
- Track recovery in AR reports.
One clinic saw $23K per month recovered after fixing unbilled services from superbill review. This method plugs revenue leaks from undercoding or service mapping errors. It improves charge master accuracy over time.
Certified coders, like CPC or CCS, lead these audits to ensure documentation improvement. Practices avoid revenue cycle gaps by adding this to monthly workflows. Expect better net collection percentages with regular checks.
Denial Management Analysis
Systematic denial analysis recovers 65% of write-offs via root cause trending. Billing services categorize denials by payer and code, such as CO-97 for service not covered. They spot patterns in claim denials from rejected claims or timely filing issues.
Key workflow steps include:
- Categorize by payer and denial code from remittance advice.
- Trend top 10 reasons with billing analytics.
- Build appeals templates for common issues like prior authorizations.
- Track success rates and adjust the scrubbing process.
A practice cut CO-97 denials 82% by tightening the auth process and patient eligibility checks. This reduces write-offs and boosts reimbursement optimization. Focus on root cause analysis for lasting fixes.
Integrate denial management into revenue cycle management for fewer billing errors. Use EOB analysis to handle secondary claims and appeals process effectively. Medical practices see faster cash flow from these targeted efforts.
AR Aging Report Scrutiny
Claims over 90 days represent 43% recoverable revenue when properly worked. Medical billing services break down AR aging into buckets: 0-30 days gets 10% effort, 31-60 days 25%, 61-90 days 35%, and 90+ days 30%. This prioritizes high-impact areas.
For 0-30 days, confirm clean claims and patient payments like copays. In 31-60, resubmit corrected claims and follow up on payer rules. For 61-90, escalate appeals and check for unposted payments.
Over 90 days needs deep work: payer contract reviews, late charge capture, and bad debt assessment. Aim for less than 10% in the over 90 bucket as a benchmark. Strategies include staff training on billing workflow and automation tools.
Track days in AR and cost per claim as KPIs. This scrutiny finds hidden revenue from duplicate claims or voided claims. Practices improve financial reconciliation and month-end close with these habits.
Payer Contract Compliance Reviews
Annual contract modeling reveals 8-15% underpayments per payer. Services extract fee schedules from payer contracts and model expected reimbursements. They compare against actual payments received to flag discrepancies.
Run this 4-step contract audit:
- Extract fee schedules for CPT and HCPCS codes.
- Model reimbursements based on contract terms.
- Compare to payments from EOBs and ERA.
- Calculate underpayments and pursue recovery.
One group discovered $187K in Blue Cross underpayments over 18 months through this check. It catches issues like bundle payments or fee schedule changes. Regular reviews keep payer reimbursements correct.
Include Medicare billing and Medicaid rules in these audits for full coverage. Certified coders verify ICD-10 and modifier use to support claims. This builds revenue integrity and prevents future leaks.
Case Studies of Detected Leaks
Real recoveries from 3 practices show exactly how leaks were found and fixed. Multi-specialty groups recovered $450K combined through targeted revenue cycle management. Detailed steps reveal replicable processes any medical practice can apply.
Medical billing services used billing analytics and certified coders with CPC certification to spot issues like undercoding and missing modifiers. These groups faced common problems such as claim denials, unposted payments, and AR management challenges. Fixing them improved cash flow and practice profitability.
One key approach involved scrubbing processes and front-end processes before claim submission. Practices saw quick wins in AR aging and denial management. Such tactics help identify revenue leaks hidden in daily billing workflows.
Outsourced RCM teams brought fee schedule audits, payer contract reviews, and revenue cycle audit expertise. Results included better reimbursement rates and fewer rejected claims. Practices gained actionable insights for ongoing revenue assurance.
Recovering Lost Modifier Revenue

Cardiology practice recovered $156K by adding -59 modifier and proper surgical coding to 2,847 PCI procedures. The group with 15 docs had only 18% modifier capture due to coding inaccuracies. Medical billing services stepped in with an algorithm to flag eligible claims.
Coders reviewed flagged cases for proper use of CPT codes, ICD-10 codes, and modifiers. This caught instances where distinct procedural services went underbilled. The process fixed revenue leaks from overlooked documentation.
Implementation took a 4-week rollout with EHR integration: week one for algorithm setup, two for coder training, three for testing, and four for full launch. Monthly new revenue hit $13K. EHR integration ensured ongoing charge capture.
Practice saw improvements in net collection percentage, days in AR, and KPI metrics. Certified coders, CPC and CCS, maintained billing compliance. This method now prevents similar leaks in cardiology billing.
Identifying Bundled Service Overpayments
Ortho group identified $94K overpayments from unbundled injections across Medicare Advantage plans. NCCI edits were bypassed, leading to improper payments on bundled services. Billing services detected this through advanced scrubbing software.
Software scanned claims for HCPCS codes and global periods violating bundle rules. Review found $47 per check across 2K claims. Root cause analysis pointed to coder errors in service mapping.
Recovery involved appeals process, appeals backlog management, and refunds where needed. Prevention came via coder training on payer rules and pre-edit checks. Monthly EOB analysis now flags potential issues early.
Group reduced duplicate claims, zero pay claims, and improved financial reconciliation. Real-time reporting dashboards track KPI metrics like collection rates. This boosted operational efficiency in specialty billing.
Preventive Strategies Implemented by Services
Medical billing services shift from reactive recovery to proactive billing and prevention in revenue cycle management. They set up daily processes that keep claim denials under 2%, far better than the 15% many medical practices face. This approach spots revenue leaks early, like undercoding or missing charges, before they hit accounts receivable.
Pro services implement daily processes and back-end processes preventing 92% of common leaks proactively. They use standardized workflows tied to EHR integration and payer rules. Practices see better cash flow and fewer AR aging issues as a result.
These strategies include scrubbing processes for clean claims and regular fee schedule audits. Billing specialists track payer contracts to avoid underpayments. Over time, this builds revenue integrity and supports practice profitability.
Certified coders follow CMS guidelines, OIG guidelines, and compliance rules closely. They handle prior authorizations and patient eligibility checks upfront. This prevents rejected claims and timely filing problems common in in-house billing.
Standardized Coding Protocols
Standardized E/M coding protocols reduce coding inaccuracies that lead to denials. Medical billing services enforce strict rules using ICD-10 codes, CPT codes, and HCPCS codes. They train certified coders, like those with CPC or CCS credentials, on these daily.
List 6 coding rules reducing errors 84%: 1) Dual coder review for >$500 claims, 2) Modifier decision tree for bundles, 3) CPC/CCS-only coding staff, 4) Weekly NCCI updates checked, 5) E/M leveling rubrics applied, 6) Payer-specific guides followed. These steps catch undercoding and overcoding fast.
Services run quarterly coder calibration sessions, compliance audits, and audit 5% of claims monthly. They review superbills and encounter forms for charge capture. This keeps documentation improvement on track and supports billing compliance.
For example, in cardiology billing, they map services to the charge master accurately. Quarterly audits reveal root cause analysis for any gaps. Practices learn about revenue cycle problems this way.
Daily Claims Reconciliation
Daily claims reconciliation and claim aging keeps AR aging low and catches underpayments quickly. Medical billing services match every claim to its EOB or remittance advice. This process flags issues like unposted payments or duplicate claims right away.
Daily EOB analysis and EOB-to-claims matching catches 91% of underpayments within 72 hours. Here’s the 7-step daily workflow: 1) Pull EOBs from all payers, 2) Auto-match claims via billing software, 3) Flag variances >5%, 4) Post AR accurately, 5) Launch underpayment appeals, 6) Update performance dashboards, 7) Generate weekly summary reports.
Billing specialists handle EOB analysis and ERA posting for Medicare billing, Medicaid billing, and commercial insurance. They check copays, deductibles, and coinsurance postings. This prevents revenue leakage from self-pay accounts or bad debt write-offs.
With EHR integration and practice management software, reconciliation ties into real-time reporting. Services track KPI metrics like days in AR and collection rates. Practices end up with smoother month-end close and better financial reconciliation.
Benefits of Outsourcing Billing
Medical practices that outsource billing to specialists gain more than just better revenue capture and revenue collection. They get compliance peace of mind and free up physician time for patient care. Beyond fixing revenue leaks like claim denials and unposted payments, outsourced services handle the full revenue cycle management.
Practices outsourcing see 22% net revenue increase within 6 months and better revenue forecasting, according to KSM Consulting. This comes from spotting billing errors, undercoding, and missing charges that in-house teams often miss. Cash flow improves as days in AR drop and clean claims rise.
Physicians reclaim hours lost to chasing payer reimbursements or appeals. Certified coders with CPC and CCS credentials ensure accurate ICD-10, CPT, and HCPCS codes. This setup boosts practice profitability without the hassle of in-house billing staff training.
Industry benchmarking shows a 9% collection rate improvement and better billing KPIs on average. Clinics see faster month-end closes and reliable revenue forecasting. Outsourcing also covers EHR integration for smooth charge capture and denial management.
Quantifiable ROI from Leak Prevention
AR days reduces from 52 to 34 while boosting net collection from 94% to 99%. Medical billing services identify revenue leaks like undercoding and unposted payments through scrubbing processes. This leads to quick wins in reimbursement optimization.
Consider a typical ROI: Year 1 revenue gain of $185K against costs of $72K yields 157% return. Metrics improve with days in AR dropping 18 days, AR management, clean claim rate up 24%, and collection rate rising 5%. Sarah’s 8-provider family practice jumped from $2.1M to $2.6M in collections after switching.
These gains come from fixing root causes like timely filing issues and duplicate claims. Billing specialists review remittance advice and EOB analysis daily. Practices track KPI metrics such as cost per claim to measure ongoing success.
Real-time dashboards show AR aging and denial trends. This helps with payer contract audits and fee schedule reviews. Outpatient clinics and specialty billing areas like cardiology see the biggest lifts in hidden revenue recovery.
Compliance and Audit-Ready Reporting
Automated audit trails and revenue cycle audit trails satisfy 100% of CMS/OIG requests within 24 hours. Medical billing services provide HIPAA-compliant dashboards and HIPAA billing for tracking coding inaccuracies and overcoding risks. This keeps practices audit-ready and avoids fraud prevention penalties.
Key compliance deliverables include:
- Daily claim edit logs to catch rejected claims early.
- Coder productivity reports from certified coders.
- Denial trending dashboards for root cause analysis.
- Payer underpayment summaries with appeals process support.
- RAC audit prep packages for financial audits.
These tools make sure billing follows Medicare and Medicaid rules. Practices get concrete information on patient eligibility and prior authorizations. This setup supports revenue integrity across commercial insurance and self-pay accounts.
For example, a HIPAA-compliant dashboard flags unbilled services and late charges instantly. Monthly reports cover copays, deductibles, and bad debt write-offs. This prepares multi-location practices for OIG compliance checks without stress.
About the Author
Ethan Cole is a business growth advisor and serial entrepreneur with over two decades of hands-on experience helping startups and small businesses thrive. With a background in finance and operations, he’s led multiple companies from early-stage concepts to multi-million-dollar exits. Ethan specializes in scaling strategies, cost reduction, and building systems that support sustainable growth. As a content contributor for Kwote Advisor, he shares practical insights to help business owners make smarter decisions when launching, managing, and expanding their ventures.